Peter Attia’s Quest to Live Long and Prosper
Some of my earliest memories are of summers with my grandparents, in New Delhi. I spent long, scorching months drinking lassi, playing cricket, and helping my grandparents find ripe mangoes at roadside markets. Then I’d return to the U.S., my English rusty from disuse, and go months or years without seeing them. At some point, my India trips started to feel like snapshots of loss. My grandfathers died suddenly, probably of heart attacks. My Biji, my father’s mother, fell and broke her hip in her seventies, and she spent her last years moving back and forth between her bed and her couch. My Nani, my mother’s mother, developed excruciating arthritis in both knees; in order for her to leave her fifth-floor walkup, my uncle practically had to carry her down the stairs. I have always wondered whether their fading vitality—the way their worlds contracted and their possibilities vanished—was an inevitability of aging or something that could have been averted.
Many of us have come to expect that our bodies and minds will deteriorate in our final years—that we may die feeble, either dependent or alone. Paradoxically, this outcome is a kind of success. For most of history, humans didn’t live long enough to confront the ailments of old age. In 1900, a baby born in the U.S. could expect to live just forty-seven years, and one in five died before the age of ten. But twentieth-century victories against infectious diseases—in the form of sanitation, antibiotics, and vaccines—dramatically extended life spans, and today the average newborn lives to around seventy-seven. Lately, though, progress has slowed. In the past six decades, medicine has added about seven years to the average life span—less by saving young lives than by extending old ones, and often in states of ill health. In many cases, we’re
$1.3B contract for new hospital that will improve health care in Mississauga and Toronto

A largest-in-Canada, $1.3-billion contract has been awarded to build a new hospital on the Etobicoke-Mississauga border that’s expected to significantly improve health care for people in both cities when it opens in five years.
Mississauga-based EllisDon will build the new Gilgan Family Queensway Health Centre in Etobicoke, Ontario Premier Doug Ford announced today.
Ford said the $1.3-billion contract represents Canada’s largest health infrastructure renewal project, which is being funded largely by the province via Infrastructure Ontario.
Work began this past February and the new hospital, which is part of the Trillium Health Partners health-care network that also includes Mississauga and Credit Valley hospitals, is expected to open in late 2029, officials said.
The new hospital will serve the rapidly growing needs of fast-growing communities, now and in the future, Ford noted, saying it’s “a critical step in making care more connected and convenient in Etobicoke and neighbouring communities.”
When completed, the 600,000-sq.-ft. Gilgan Family Queensway Health Centre will include a new patient tower described as a modern nine-story facility with more than 350 beds and fully private patient rooms to ensure privacy and enhance infection prevention control.
“The expanded space will also allow THP to connect more people to specialized care, including complex continuing care and rehabilitation services,” the province’s deputy health minister, Sylvia Jones, said in a news release.
“With this new hospital expansion, our government is ensuring the needs of Peel Region and Etobicoke will be met for decades to come.”
THP president and CEO Karli Farrow described the undertaking as an “historic project” that will serve the community for many generations to come.
“Once completed, the Gilgan Family Queensway Health Centre will…allow us to increase our hospital’s capacity to provide quality health care from Milton to Toronto,” she said. “This milestone
Seizing Opportunities and Revolutionizing Care with Public-Private Partnerships and Government Initiatives


Global Digital Health Market
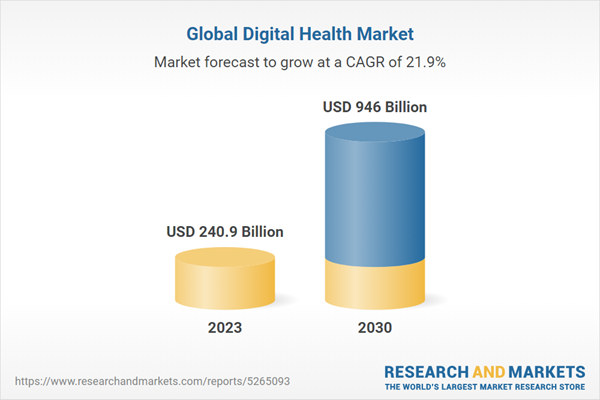
Dublin, April 11, 2024 (GLOBE NEWSWIRE) — The “Global Digital Health Market Size, Share & Trends Analysis Report by Technology (Healthcare Analytics, mHealth), Component (Hardware, Software, Services), Application, End-use, Region, and Segment Forecasts, 2024-2030” report has been added to ResearchAndMarkets.com’s offering.
The global digital health market size is anticipated to reach USD 946.0 billion by 2030 and it is projected to grow at a CAGR of 21.9% from 2024 to 2030
The market growth driven by various factors. These include the proliferation of smartphones, advancements in internet connectivity, the development of IT infrastructure, increasing healthcare IT expenditures, overburdened healthcare facilities, a growing shortage of healthcare providers, rising demand for remote patient monitoring services, escalating medical costs, improved accessibility of virtual care services, and the increasing prevalence of chronic diseases.
This growth is further propelled by the ongoing trend of digitalization in healthcare. This trend finds support in expanding public-private partnerships, emerging startups in the healthcare sector, and favorable initiatives undertaken by governments to promote digital health solutions.

Digital health encompasses diverse technologies such as telehealth services, health information technology, and mobile health (mHealth) to enhance communication within healthcare systems, fostering improved interactions between doctors and patients. The relevance of digital health technology has grown significantly, especially during the COVID-19 pandemic. These contemporary solutions enhance the patient-doctor relationship and extend preventive disease strategies. Furthermore, they contribute to a shift in healthcare towards value-based treatment, amplifying the accessibility of health information for both patients and healthcare providers.
Furthermore, integrating wearable devices into healthcare reshapes how individuals manage their health. Wearables like fitness trackers and smartwatches enable continuous monitoring of vital signs, physical activity, and other health metrics. This real-time data empowers individuals to take a proactive role in their well-being and allows
Italian Fashion Designer Roberto Cavalli Has Died at 83
Roberto Cavalli, the Italian designer who infused the print-led boho look with sex appeal, has died at 83. His passing was confirmed by the brand. “The Roberto Cavalli company shares condolences with Mr. Cavalli’s family. His legacy remains a constant source of inspiration,” said Roberto Cavalli’s CEO Sergio Azzolari.
By the time shows started to go digital (circa 2000), Cavalli was a well-established golden name in fashion; an elder, even, enjoying a second round of renown. He exuded Hefner vibes (minus the robe) when he took his fall 2001 bow smoking a pipe. (The designer was in fact asked to redesign the Playboy bunny costume in 2005.) By then the leonine Cavalli was living the good life, something that he achieved with braggadocio and brain power—and against the odds. In the context of Cacvalli’s life story, the body worship and forthright sexiness of his work, could be seen more broadly as an affirmation of life itself, which, from a young age he understood to be fragile.
Born in Florence in 1940, Cavalli’s maternal grandfather was a member of the Macchiaioli group of Italian Impressionists. His father, an anti-fascist who is thought to have been a mine surveyor, was shot by the Nazi forces when Cavalli was just three years old. The psychological impact was expressed physically through a stutter. “It was not easy for me to speak, the shock,” the designer told Luke Leitch in a 2011 interview. To support the family, his mother started sewing at home, taking in seamstresses to help her. At 17, a confident Cavalli enrolled at the Academy of Art in Florence to study art and architecture. There he met and fell in love with his first wife and the mother of two of his children, Silvanella Giannoni.
In 1960, after hand-painting some sweaters
UofA medical student champions advocacy committee to talk health care
Article content
When the province’s budget 2024 was announced, Sana Samadi said through the Alberta Medical Association’s “Urgency is Real” campaign she saw how many physicians were talking about the lack of adequate funding for health care across the province.
Seeing how physicians were bringing further awareness to the current failings of primary care was part of what influenced Samadi, a first-year medical student at the University of Alberta, to focus on the work being done at a new student committee she championed in partnership with the AMA.
Article content
Samadi, who is the president of the AMA medical student advocacy committee, launched the group in January 2024. She said the purpose of the committee is to help medical students across the province become more involved in what is happening on the ground in the health care field.
“I viewed this from a medical school perspective — students’ perspective. Even though (my peers) are interested in family medicine and they see the crisis of family medicine, they may not want to choose family medicine because of the current state,” Samadi said.
“Why would you want to join a system that you can see is having a lot of trouble right now? We need to improve this state for the years to come so that when we do enter the workforce in three to four years in our residency years, people want to choose family medicine and not only choose family medicine but choose family medicine in Alberta as opposed to other more competitive provinces like B.C.”
Samadi said while many of her fellow students are aware of the struggles in the field, there remains a gap in how they could provide their input as current students and help advocate for the health care field. On a day-to-day basis, students are
What ‘Nutrition Facts’ Labels Leave Out
The tech industry has a new trend: adopting “transparency labels” modeled after the iconic Nutrition Facts panel found on food packaging. In 2020, Apple introduced “Privacy Labels” aimed at disclosing how apps handle user data. And that was just the beginning. Starting on April 10, the FCC is requiring internet service providers to feature “Broadband Facts” labels detailing pricing, speeds, and data caps. Meanwhile, some policymakers and industry analysts have called for an “AI Nutrition Facts” label to clarify how artificial intelligence systems create content.
This rush to emulate the Nutrition Facts panel underscores the label’s status as the go-to model for consumer transparency. Yet, the history of how it achieved that status reveals the power — and the limitations — of using such labels as a regulatory tool. They can inform consumers, but they may also forestall more serious regulation that is necessary to adequately safeguard the public interest.
In the 1950s and 1960s, the Food and Drug Administration (FDA) debated the proper way to safeguard consumers from misinformation and fearmongering in health food markets. Initially, officials resisted nutrition labeling on food, seeing it as unnecessary “quackery” or the purview of medical specialists treating the ill.
But increasingly, the FDA had to weigh the growing legitimate medical interest in using diet as a preventative solution to public health, as well as the rise of a new self-improvement culture that made Americans more health conscious. FDA officials were also cognizant of declining public trust in the government’s ability to make decisions for consumers about their private lives after years of scandals. This shifted officials’ thinking and they began to accept that Americans had the right — and perhaps even the need — to seek out health information for food. They saw informative labels as empowering consumers to make choices
How To Organize A Clothing Swap
All you need to get started is clothes you’re willing to part with—and an open mind about what you might find.

Annette Nguyen founded the Shwap Club, a unique clothing-swap members club in Montreal. (Photo: Sylvie Li)
Clothing swaps are not a new concept, but with so many of them popping up all over the country, we took notice. Not only are they fun, they also allow you to give new life to your wardrobe without spending a ton of money (or, in many cases, any money at all). All you need to get started is clothes you’re willing to part with—and an open mind about what you might find.
In Montreal, the Shwap Club is formalizing the swapping process. Members bring in gently used, still-trendy pieces in order to receive store credits to “buy” other pre-loved garments.
Unlike traditional swaps, the club has two bricks-and-mortar locations and charges a per-visit ($22) or yearly fee ($145), which allows people to trade and shop as well as save any unused credits for future shopping trips if they don’t immediately find something to swap their items for. Clothing racks are stocked with brands like Aritzia, Banana Republic, Lululemon and Frank And Oak, which are favourites of the young professional client base.
Founder Annette Nguyen, a former lawyer, opened the club’s first location in 2018, having been inspired by her own attempts to keep her business-casual wardrobe fresh. “I felt like I always needed to have a new blouse and new trousers as well as fun dresses for happy hour,” she says. “Even shopping second-hand, it was getting expensive.”
After becoming a mom and experiencing how quickly children grow out of their clothes, Nguyen expanded her business beyond the nine-to-five crowd and opened a second location dedicated entirely to maternity and kids.
Swapping
Horizon’s target for reduced ER wait times is 4 times national guideline
Horizon Health Network is working to reduce emergency department wait times, with a special focus on urgent cases like Darrell Mesheau, who died in 2022 after he waited seven hours to see a doctor at the Fredericton hospital’s ER, a coroner’s inquest heard earlier this week.
Susan McCarron, clinical director of Horizon’s emergency departments in the Fredericton region, testified the goal is to get wait times for patients triaged as being Level 3 down to 120 minutes or less this year.
She did not specify if she was referring to the the Dr. Everett Chalmers Regional Hospital, all Fredericton region hospitals, or all Horizon hospitals — and Horizon did not respond to requests to clarify.
Either way, Horizon’s objective is at least four times longer than the national guideline. The Canadian Emergency Department Triage and Acuity Scale calls for Level 3 patients to be seen by a doctor within 30 minutes.
Patients assessed at this level have “conditions that could potentially progress to a serious problem requiring emergency intervention,” according to the guidelines.
These can include everything from head injury and chest pain, to asthma and vomiting, the guidelines indicate.

Level 3 patients “represent most of the patients presenting for care to the emergency department,” according to Horizon’s performance dashboard.
Horizon spokesperson Kris McDavid told CBC News no one was available for an interview and did not provide any comments about why its target wait time for Level 3 patients is so much longer than the national guideline or how it was set.
According to a trends chart on Horizon’s performance dashboard website, the last time Level
Ontario NDP wants audit into clinics charging for primary health care
Article content
Ontario’s New Democratic Party is calling on the province’s auditor general to investigate the growing number of clinics that are charging fees for primary health care.
In recent months, there has been a proliferation of private clinics offering primary care by nurse practitioners for a fee. That is leaving some of the 2.3 million Ontario residents who don’t have family doctors facing financial barriers to primary healthcare, party leader Marit Stiles said.
Article content
“We are calling for a special audit. Anyone charging patients for health care should be held accountable, full stop,” Stiles said.
The province’s auditor general, Shelley Spence, would be required to do such an audit this year if requested by the public accounts committee. The NDP health critic, France Gélinas, put such a motion before the committee on Monday, but the motion was voted down.
Such special audits have been done in the past. Last August, the auditor general released a special report on changes to the Toronto-area Greenbelt, which had been requested by all three opposition party leaders.
Stiles said the issues were both important and timely.
“I think Ontarians deserve to know exactly how widespread this issue is,” Stiles told a news conference. “Our system is built on the principle that you should not have to pay for health care.”
A number of fee-based nurse practitioner clinics have opened in Ottawa and eastern Ontario in recent months as growing numbers of area residents have lost their family physicians.
The South Keys Health Centre on Bank Street began charging patients $400 last year to access nurse practitioners. Other clinics with similar, and higher, access fees have also opened in the region. And, earlier this year, a patient at an Appletree clinic in Ottawa, who needed a routine cancer screening test after receiving a
How to spot health misinformation online
In a tech-driven world with news just at our fingertips, it can be hard to determine what’s true and what’s false.
Of all of the misinformation floating online, fake health news can be particularly dangerous, especially if it promotes things like products that actually shouldn’t be consumed.
45% of adults surveyed by KFF in 2023 reported that they’ve heard, and believe, at least one of five false claims about Covid-19 and vaccines that KFF asked them about, prior to being surveyed. One of the incorrect claims was that ivermectin can effectively treat Covid-19, and 34% of those polled believed that it was probably true or definitely true.
“It just is a matter of taking time,” says Dr. Seema Yasmin, director of the Stanford Health Communication Initiative at Stanford University. Yasmin is also the author of “What The Fact?!: Finding the Truth in All the Noise.”
“And so often when we see people fall for false information, they just haven’t taken even a second to do some of these basic checks.”
Here are a few indicators that a post online is spreading health misinformation, according to Yasmin and Deen Freelon, professor at the Annenberg School for Communication at the University of Pennsylvania.
4 signs of health misinformation online
1. It sounds too good to be true
“If something sounds too good to be true, then do a little bit more investigating,” Yasmin says.
Question the credibility of new health information that uses “words like cure, 100% effective [and] guaranteed. You’d be surprised at how quickly the human brain can want to fall for those false promises,” she adds.
“You want to do extra digging when those kinds of big promises are attached to a product or something that somebody is selling.”

















